Fill a Valid Tb Test Template
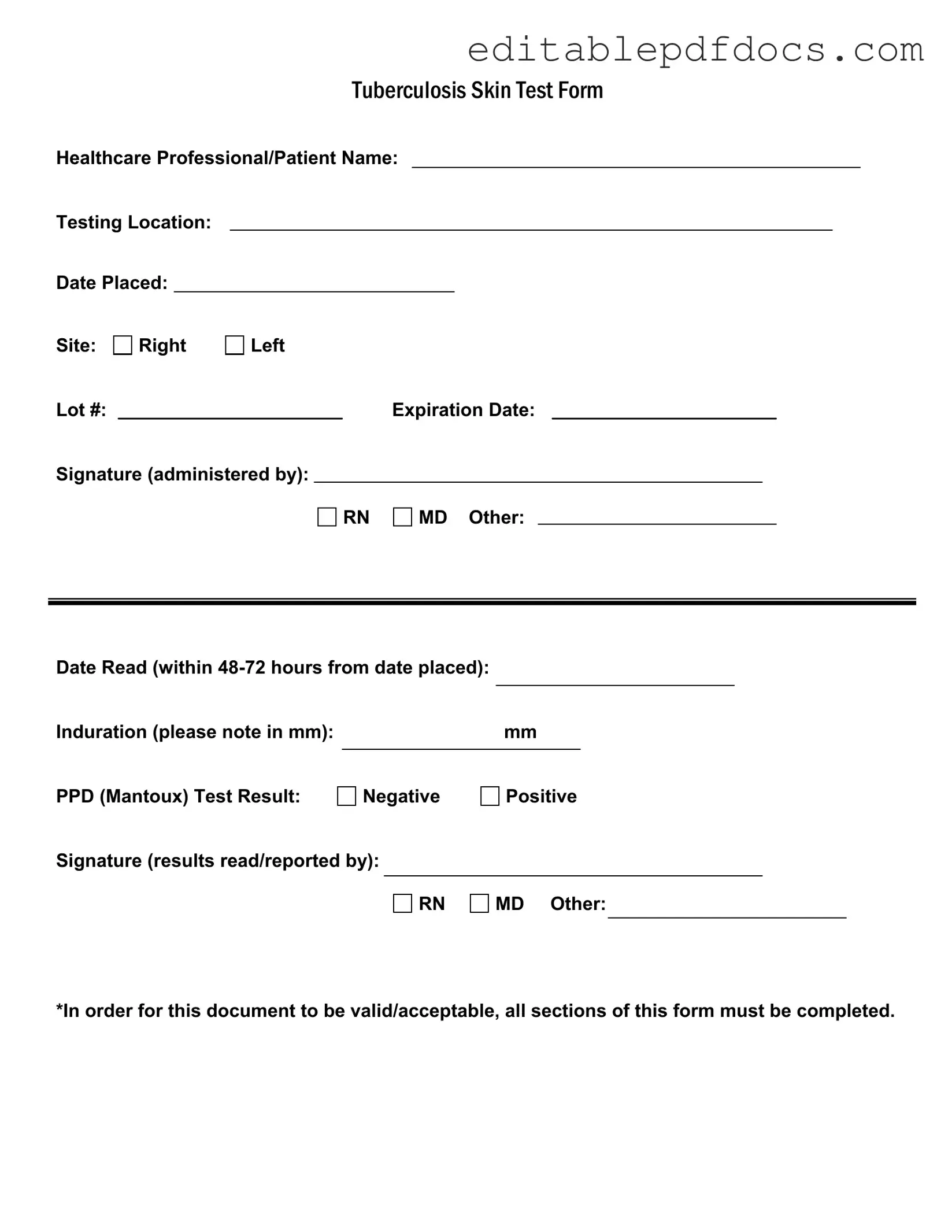
The Tuberculosis (TB) Skin Test Form serves as a crucial document for healthcare professionals and patients alike, ensuring that the TB screening process is thorough and well-documented. This form captures essential information, beginning with the names of the healthcare professional and patient, alongside the testing location and the date the test was placed. It specifies the site of the test, whether on the right or left arm, and includes important details such as the lot number and expiration date of the testing material. The signature of the administering professional—whether a registered nurse, medical doctor, or other qualified personnel—validates the process. Following the test, the form requires a reading of the results within 48 to 72 hours, noting the induration measurement in millimeters. This measurement determines whether the PPD (Mantoux) test result is negative or positive. Finally, the form must be signed by the professional who reads and reports the results, ensuring accountability and accuracy. It is imperative that all sections of this form are completed for it to be considered valid and acceptable in medical settings.
Document Details
| Fact Name | Description |
|---|---|
| Form Purpose | The Tuberculosis Skin Test Form is used to document the administration and results of the PPD (Mantoux) test. |
| Completion Requirement | All sections of the form must be completed for the document to be valid and acceptable. |
| Reading Timeline | The test results must be read within 48 to 72 hours after placement for accurate assessment. |
| Governing Law | State-specific requirements for tuberculosis testing may be governed by public health laws, such as the CDC guidelines and state health department regulations. |
Dos and Don'ts
When filling out the TB Test form, it’s crucial to be thorough and accurate. Here’s a list of things you should and shouldn’t do to ensure your form is completed correctly.
- Do ensure all sections of the form are completed.
- Do write legibly to avoid any misinterpretation of your information.
- Do double-check the testing location and date placed for accuracy.
- Do specify the site of the test clearly (right or left).
- Do include the lot number and expiration date of the PPD.
- Don’t leave any section blank; incomplete forms may not be accepted.
- Don’t forget to sign the form where required.
- Don’t use abbreviations that might confuse the reader.
- Don’t submit the form without confirming the results have been read and reported.
By following these guidelines, you can help ensure that your TB Test form is processed smoothly and efficiently.
Documents used along the form
The Tuberculosis (TB) Test form is essential for documenting the administration and results of the TB skin test. However, several other forms and documents are commonly used in conjunction with it. These documents help ensure comprehensive patient care and compliance with health regulations.
- Patient Medical History Form: This form collects information about the patient's past medical conditions, allergies, and family history. It aids healthcare providers in understanding the patient's overall health and any potential risks associated with the TB test.
- Informed Consent Form: Before administering the TB test, healthcare professionals often require patients to sign an informed consent form. This document ensures that patients understand the procedure, its purpose, and any potential risks involved.
- TB Screening Questionnaire: This questionnaire is used to assess the patient's risk factors for tuberculosis. It typically includes questions about exposure history, travel, and symptoms, helping healthcare providers determine the necessity of the TB test.
- Emotional Support Animal Letter: This document plays a crucial role for individuals who require the support of their emotional support animals. By obtaining this letter from a licensed mental health professional, individuals can confirm the importance of their animal's companionship in their mental health journey. For more information about this letter, visit Fillable Forms.
- Follow-Up Evaluation Form: If the TB test result is positive, a follow-up evaluation form is necessary. This document details further testing and treatment plans, ensuring that the patient receives appropriate care.
- Immunization Record: This record provides a comprehensive overview of the patient's vaccination history. It may be relevant in evaluating the patient's immunity and overall health status in relation to TB exposure.
- Referral Form: In cases where a patient requires additional evaluation or treatment, a referral form is often completed. This document facilitates communication between healthcare providers and ensures that the patient receives specialized care as needed.
These forms and documents play a crucial role in the TB testing process. They not only support the accurate documentation of patient information but also enhance the quality of care provided. By ensuring all necessary paperwork is completed, healthcare professionals can better manage patient health and safety.
Popular PDF Forms
Can One Parent Take a Child on a Cruise Royal Caribbean - The form captures essential information for contact in case of emergencies.
The Employment Verification Form is a crucial document designed to confirm an individual's employment status and history. It serves as a key resource for potential employers, lenders, and other entities needing to verify a person's work background. To make the process easier, you can find more information and access this form at PDF Documents Hub. Understanding and filling out this form accurately is essential, so take a moment to ensure you’re ready to complete it by clicking the button below.
Affidavit of Death of Joint Tenant - Critical for beneficiaries wanting to claim their interests.
Custody Affidavit - It underscores that the relinquishment may not be easily reversible beyond a set timeframe.
Similar forms
The Tuberculosis (TB) Test form shares similarities with several other healthcare-related documents. Here are eight documents that exhibit comparable features:
- Vaccination Record: Like the TB Test form, a vaccination record includes patient information, the date of administration, and the signature of the healthcare professional who administered the vaccine.
- Medical Power of Attorney: For crucial health care directives, consider our essential Medical Power of Attorney form details to ensure your medical preferences are honored when you cannot communicate them yourself.
- Medical Clearance Form: This document requires patient identification, the purpose of the clearance, and the healthcare provider's signature, similar to the TB Test form's need for completion and signature by a professional.
- Consent Form: A consent form outlines the procedure being performed, patient details, and requires a signature, just as the TB Test form necessitates signatures and patient information.
- Patient History Form: This form collects patient demographics and medical history, similar to how the TB Test form gathers patient and testing information.
- Referral Form: A referral form typically includes patient details and the reason for the referral, akin to the TB Test form's requirement for comprehensive patient data.
- Lab Test Requisition: This document requests specific lab tests and includes patient information, much like the TB Test form requires details about the patient and the test conducted.
- Emergency Contact Form: An emergency contact form contains patient information and contact details, paralleling the TB Test form's need for personal data and signatures.
- Health Assessment Form: This form gathers information about a patient's health status and includes sections for signatures, similar to the TB Test form's comprehensive approach to documenting patient data.
Common mistakes
When filling out the Tuberculosis (TB) Test form, many people make common mistakes that can lead to delays or complications. One frequent error is leaving out important personal information. The form requires your name and the name of the healthcare professional. Omitting these details can render the form incomplete.
Another mistake is not specifying the testing location. This section is crucial for tracking the test and ensuring that results are properly attributed. Without this information, it may be difficult for healthcare providers to verify the test.
Many individuals also forget to include the date placed and the date read. These dates are essential for determining the validity of the test results. Remember, the test must be read within 48 to 72 hours of placement, so accurate dates are necessary.
Some people mistakenly check the wrong site for the test placement. It’s important to indicate whether the test was done on the right or left arm. This detail helps healthcare providers know where to look for the induration.
Another common oversight is neglecting to record the induration measurement in millimeters. This measurement is vital for interpreting the results. If it’s missing, the healthcare provider may not be able to determine whether the test result is positive or negative.
Individuals sometimes forget to note the lot number and expiration date of the PPD solution used. These details are important for quality control and ensuring that the test is valid. Without them, the results may be questioned.
When it comes to signing the form, some people fail to provide the signature of the healthcare professional who administered the test. This signature is a key part of the documentation process and ensures accountability.
Another mistake is not indicating who read the results. The form requires the signature of the person who interpreted the test results, whether it’s an RN, MD, or another qualified individual. This step is critical for maintaining the integrity of the results.
People may also overlook the requirement that all sections of the form must be completed. Incomplete forms are often rejected, which can lead to unnecessary delays in receiving test results.
Finally, it’s essential to double-check the entire form before submission. Simple typos or errors can lead to confusion. Taking a moment to review the form can save time and ensure that the test results are processed smoothly.