Fill a Valid Progress Notes Template
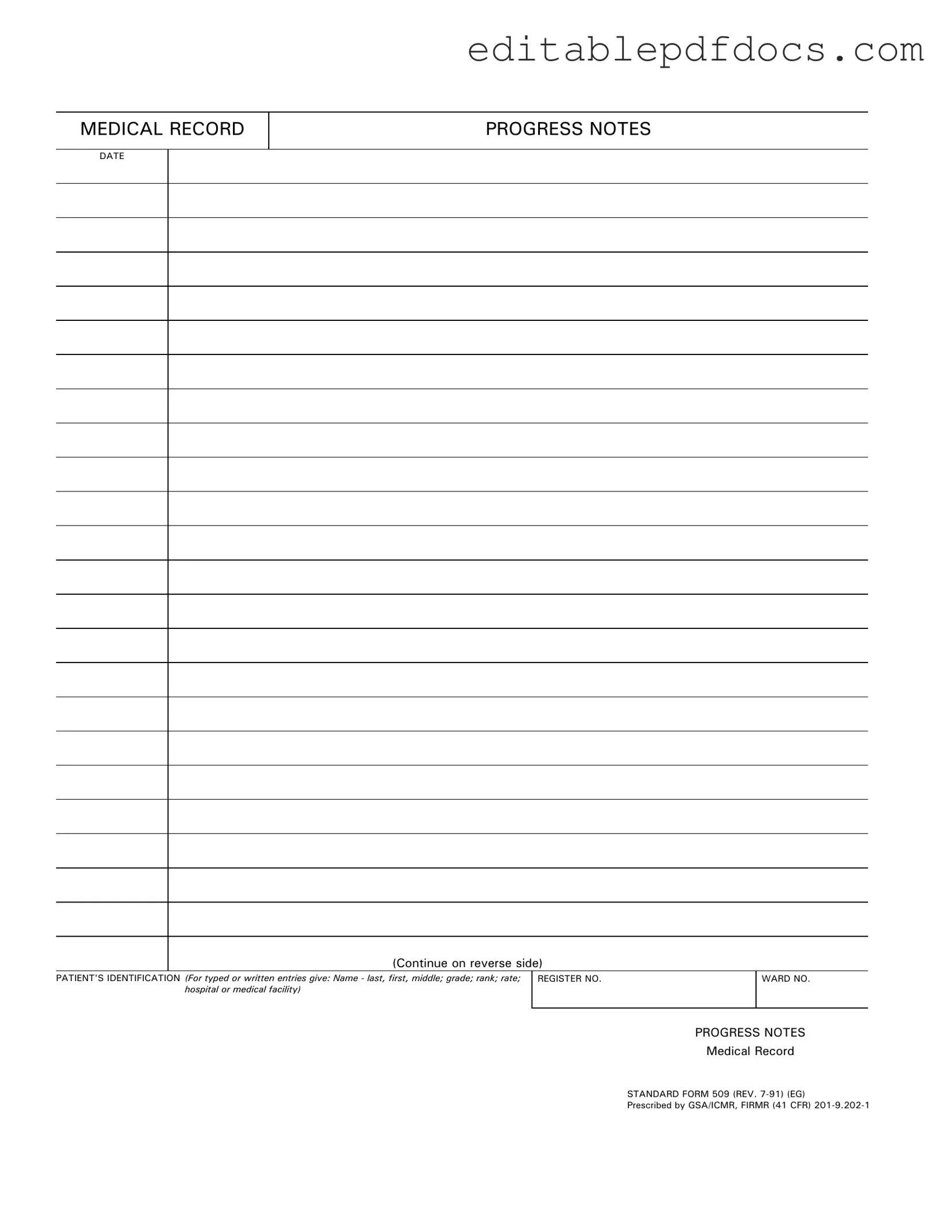
The Progress Notes form serves as a vital component in the medical record-keeping process. This form is designed to document important information regarding a patient's treatment and progress during their stay at a medical facility. It includes essential details such as the patient's identification, which encompasses their name, grade, rank, and the hospital or medical facility where they are receiving care. Each entry must be dated to ensure a clear timeline of the patient's treatment history. The form is standardized, identified as Standard Form 509, and has undergone revisions to maintain compliance with regulations. Accurate completion of the Progress Notes form is crucial, as it not only reflects the ongoing care provided to the patient but also serves as a legal record of the medical services rendered. This documentation is essential for continuity of care and can be referenced by various healthcare professionals involved in the patient's treatment.
Document Details
| Fact Name | Description |
|---|---|
| Purpose | The Progress Notes form is used to document patient care and treatment in medical records. |
| Identification | It requires patient identification, including name, grade, rank, and hospital or medical facility. |
| Standardization | This form is a standardized document, specifically Standard Form 509 (REV. 7-91). |
| Governing Laws | It is prescribed by GSA/ICMR and governed by FIRMR (41 CFR) 201-9.202-1. |
| Revision Date | The current version of the form was revised in July 1991. |
| Back Side Usage | There is an option to continue notes on the reverse side of the form. |
| Record Keeping | Progress Notes are essential for maintaining accurate medical records and continuity of care. |
| Compliance | Using this form helps ensure compliance with federal regulations regarding medical documentation. |
Dos and Don'ts
When filling out the Progress Notes form, it's essential to follow specific guidelines to ensure accuracy and clarity. Here are nine things you should and shouldn't do:
- Do enter the date clearly at the top of the form.
- Do provide complete patient identification, including name, grade, rank, and medical facility.
- Do use legible handwriting or type the entries to avoid confusion.
- Do keep your notes concise and focused on relevant medical information.
- Do ensure that the information is accurate and up-to-date.
- Don't leave any sections of the form blank unless instructed otherwise.
- Don't use abbreviations that could be misunderstood.
- Don't include personal opinions or irrelevant information in the notes.
- Don't forget to sign and date the form after completion.
Documents used along the form
When managing patient records, several forms and documents work in tandem with the Progress Notes form. Each of these documents serves a specific purpose in ensuring comprehensive patient care and accurate record-keeping. Below is a list of commonly used forms alongside a brief description of each.
- Patient Intake Form: This form collects essential information about a new patient, including their medical history, current medications, and contact details. It helps healthcare providers understand the patient's background and needs.
- Job Application Form: Prospective employees can utilize the Fillable Forms to complete their applications for positions within Chick-fil-A, ensuring they provide all necessary personal information and work history to boost their chances of employment.
- Consent for Treatment: This document ensures that patients agree to receive medical treatment. It outlines the procedures involved and any potential risks, ensuring patients are informed before proceeding.
- Referral Form: When a patient needs to see a specialist, a referral form is used. It includes details about the patient's condition and the reason for the referral, facilitating communication between providers.
- Medication Administration Record (MAR): This form tracks the medications given to a patient, including dosages and administration times. It helps prevent errors and ensures that patients receive their medications as prescribed.
- Discharge Summary: After a patient leaves a medical facility, a discharge summary is created. It summarizes the patient's treatment, progress, and any follow-up care needed, ensuring continuity of care.
- Lab Results Report: This document provides the results of any laboratory tests performed on the patient. It includes important information that can influence treatment decisions and patient care.
- Care Plan: A care plan outlines the specific goals and interventions for a patient's treatment. It is tailored to the individual needs of the patient and helps guide healthcare providers in delivering care.
These forms are essential for maintaining accurate and effective patient records. Together, they help healthcare providers deliver the best possible care while ensuring compliance with regulations and standards.
Popular PDF Forms
Scrivener's Affidavit California - The Scrivener's Affidavit serves as a safeguard for all parties in a transaction.
Completing the New York MV-51 form accurately is essential to ensure a smooth transaction during the vehicle sale process. For those looking to access this important document, further information can be found at nyforms.com/new-york-mv51-template, which provides guidance on how to properly fill out the form and the necessary steps to take before finalizing any sale.
Cuddy Buddy Application - Enhance your self-care routine with cuddle therapy.
Broker Price Opinion Letter Pdf - Gives adjustments based on property features to arrive at adjusted sales price.
Similar forms
The Progress Notes form is a critical document in the medical field, used to track a patient's treatment and progress over time. It shares similarities with several other documents that also serve to record important information about patient care. Here are ten documents that are comparable to Progress Notes, along with a brief explanation of how they are similar:
- Patient Assessment Forms: These forms collect detailed information about a patient's condition and history, similar to how Progress Notes document ongoing observations and evaluations.
- SOAP Notes: This structured format (Subjective, Objective, Assessment, Plan) is often used by healthcare providers to capture patient encounters, much like Progress Notes do in a less formal manner.
- Room Rental Agreement: For those renting properties, the essential Room Rental Agreement resources provide clear guidelines for landlords and tenants.
- Clinical Encounter Forms: These documents summarize the details of a patient visit, including diagnosis and treatment, paralleling the information recorded in Progress Notes.
- Discharge Summaries: These summaries provide an overview of a patient's hospital stay and treatment, akin to the ongoing documentation found in Progress Notes.
- Care Plans: Care plans outline the goals and interventions for a patient’s treatment, similar to how Progress Notes track the progress toward those goals.
- Medication Administration Records (MAR): MARs document the administration of medications, reflecting the same attention to patient care as Progress Notes.
- Referral Letters: These letters communicate a patient's needs and treatment history to other healthcare providers, echoing the purpose of Progress Notes in sharing patient information.
- Treatment Plans: Treatment plans detail the strategies for managing a patient’s condition, resembling the ongoing updates provided in Progress Notes.
- Incident Reports: These reports document unusual occurrences in patient care, similar to how Progress Notes may note significant changes in a patient’s condition.
- Insurance Claim Forms: These forms require detailed information about patient treatment and care, reflecting the same thoroughness found in Progress Notes.
Common mistakes
Filling out the Progress Notes form accurately is crucial for maintaining comprehensive medical records. One common mistake is failing to include the date on the form. Without a clear date, it becomes difficult to track the timeline of a patient’s care. This oversight can lead to confusion and may impact treatment decisions.
Another frequent error involves the patient's identification. Individuals often neglect to provide complete information, such as the patient's full name, grade, rank, or rate. Incomplete identification can hinder communication among healthcare providers and may affect the continuity of care.
Many people also overlook the importance of the register number and ward number. These identifiers are essential for organizing and retrieving patient records efficiently. Omitting this information can lead to delays in accessing necessary medical history.
In addition, some individuals fail to use the correct standard form. Using an outdated or incorrect version can cause discrepancies in record-keeping and may violate institutional policies. It is important to ensure that the most current form is being utilized.
Another common mistake is the lack of detailed progress notes. Brief or vague entries do not provide adequate information for other healthcare providers. Detailed notes are essential for understanding the patient’s condition and the rationale behind treatment decisions.
People sometimes write in a way that is difficult to read. Illegible handwriting or poor formatting can lead to misinterpretations of the notes. Clear and concise writing is necessary to ensure that all team members can understand the information presented.
Some individuals may also forget to sign the form. A signature is a critical component that validates the notes and confirms the author’s accountability. Without a signature, the notes may not be considered official or may be questioned during audits.
Another mistake is not reviewing the completed form before submission. Failing to double-check for errors can lead to inaccuracies that may affect patient care. A thorough review can catch mistakes and ensure that all required information is included.
Lastly, individuals sometimes neglect to consider the confidentiality of the information being recorded. It is essential to handle patient information with care to protect their privacy. Adhering to confidentiality guidelines is not only a legal requirement but also an ethical obligation.