Fill a Valid Medication Administration Record Sheet Template
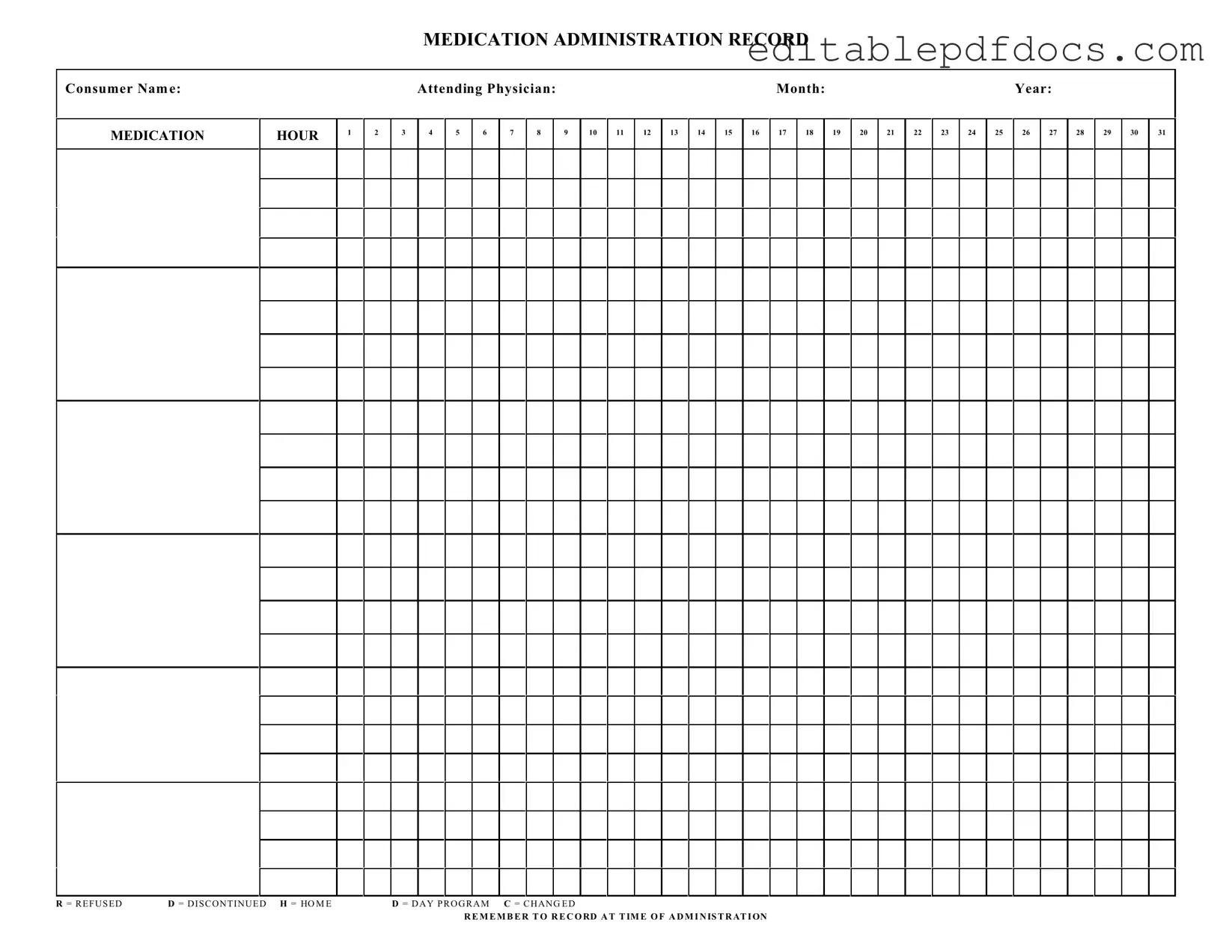
The Medication Administration Record Sheet (MARS) serves as a vital tool in the healthcare system, ensuring accurate tracking of medication administered to patients. This form is designed to capture essential information, including the consumer's name, attending physician, and the specific month and year of administration. Each hour of the day is meticulously laid out, allowing healthcare providers to document the precise time medications are given. Notably, the form includes designated areas to indicate various statuses of medication, such as "Refused," "Discontinued," or "Changed." These notations are crucial for maintaining a clear and comprehensive record of a patient’s medication regimen. By providing a structured format, the MARS enhances communication among healthcare professionals, ultimately contributing to better patient outcomes. The importance of timely and accurate documentation cannot be overstated; it is essential that all entries are made at the time of administration to ensure the integrity of the patient’s medical record.
Document Details
| Fact Name | Description |
|---|---|
| Consumer Name | The form requires the full name of the consumer receiving medication. |
| Medication Hour | Hours are designated for medication administration, ranging from 1 to 31. |
| Attending Physician | The name of the physician responsible for the consumer's care must be included. |
| Date Fields | The form includes fields for the month and year of medication administration. |
| Administration Codes | Specific codes indicate medication status: R for Refused, D for Discontinued, H for Home, D for Day Program, and C for Changed. |
| Record Keeping | It is crucial to record medication administration at the time it occurs. |
| State-Specific Regulations | In some states, this form is governed by specific healthcare regulations to ensure compliance. |
| Importance of Accuracy | Accurate completion of the form is essential for the safety and well-being of the consumer. |
Dos and Don'ts
When filling out the Medication Administration Record Sheet, it's important to be thorough and accurate. Here are some guidelines to help you navigate the process effectively.
- Do write clearly and legibly. This ensures that everyone can read the information without confusion.
- Do fill in the consumer's name and the attending physician's name accurately. This helps in maintaining proper records.
- Do record the date and month correctly. This is crucial for tracking medication administration over time.
- Do check the medication hour boxes carefully. Make sure to mark the correct time of administration.
- Don't leave any fields blank. Incomplete forms can lead to misunderstandings or errors in medication administration.
- Don't use abbreviations that may not be universally understood. Clarity is key in medical documentation.
- Don't forget to record any refusals or changes in medication status. This information is vital for ongoing care.
- Don't rush through the process. Take your time to ensure that all information is accurate and complete.
Documents used along the form
When managing medication administration, several important documents accompany the Medication Administration Record (MAR) form. Each of these documents plays a crucial role in ensuring accurate and safe medication practices. Below are some commonly used forms and their descriptions.
- Medication Order Form: This document outlines the specific medications prescribed by a physician, including dosage, frequency, and duration of treatment. It serves as the official authorization for administering medications to the consumer.
- Patient Consent Form: This form is designed to obtain consent from the patient or their legal representative before administering medication. It ensures that the patient is informed about the treatment and agrees to proceed.
- Allergy and Adverse Reaction Record: This document lists any known allergies or previous adverse reactions a patient may have experienced. It is critical for preventing potential allergic reactions during medication administration.
- Medication Inventory Log: This log tracks the quantities of medications on hand. It helps healthcare providers maintain an accurate count and manage stock levels effectively, ensuring that medications are available when needed.
- New York Certificate of Incorporation: This essential document is required for establishing a corporation in New York, providing crucial information including the corporation's name and purpose. For more details, refer to the nyforms.com/new-york-certificate-template/.
- Incident Report Form: Should any issues arise during medication administration, such as a medication error or adverse reaction, this form is used to document the incident. It is vital for quality control and improving future practices.
- Medication Discharge Summary: This summary provides information on medications the patient will continue after discharge, including instructions for use. It ensures continuity of care as the patient transitions from one setting to another.
Utilizing these documents alongside the Medication Administration Record form enhances patient safety and improves the overall effectiveness of medication management. Each form contributes to a comprehensive approach to healthcare, promoting transparency and accountability in medication practices.
Popular PDF Forms
Florida Inheritance Tax - The form asks for the decedent's name, date of death, and details regarding their domicile.
Creating a Job Application - Willingness to work overtime can be indicated with a simple yes or no.
For those interested in understanding loan agreements better, our guide on the important aspects of a Promissory Note provides valuable insights into the responsibilities and requirements outlined in these legal documents.
How Long Does a Discharge Upgrade Take - Submission timelines for the DD 149 may vary based on circumstances.
Similar forms
The Medication Administration Record Sheet (MAR) is a crucial document in healthcare settings, particularly for tracking the administration of medications to patients. Several other documents serve similar purposes, ensuring proper documentation and communication regarding patient care. Below are seven documents that share similarities with the MAR:
- Patient Care Plan: This document outlines the overall treatment goals for a patient, including medication management. Like the MAR, it requires regular updates and collaboration among healthcare providers to ensure that the patient receives appropriate care.
- Medication Reconciliation Form: This form is used to compare a patient's current medications with what they should be taking. Both documents help to prevent medication errors and ensure continuity of care.
- Nursing Progress Notes: These notes provide a detailed account of a patient's condition and responses to treatments, including medications. Similar to the MAR, they serve as a record of care and are essential for effective communication among healthcare team members.
- Physician Orders: These documents specify the medications prescribed by a physician. The MAR reflects these orders, ensuring that the medications are administered as intended, thus maintaining a clear link between the prescription and administration.
- Incident Report: When medication errors occur, an incident report is filed to document the event. Both the MAR and incident reports are vital for quality assurance and improving medication safety protocols.
- Medication Administration Policy: This policy outlines the procedures and protocols for administering medications within a healthcare facility. Similar to the MAR, it emphasizes the importance of accuracy and accountability in medication administration.
- Trailer Bill of Sale: The California Trailer Bill of Sale is a crucial document for transferring ownership of a trailer, ensuring all necessary information is documented. For a seamless transaction, consider utilizing Fillable Forms to complete the process efficiently.
- Patient Medication History: This document provides a comprehensive overview of a patient's past and current medications. Like the MAR, it plays a critical role in ensuring safe and effective medication management, particularly during transitions of care.
Common mistakes
Filling out the Medication Administration Record Sheet is crucial for ensuring that patients receive their medications safely and on time. However, many people make common mistakes that can lead to confusion or errors in medication administration. One frequent error is not writing the consumer's name clearly at the top of the form. A legible name is essential to avoid any mix-ups, especially in facilities with multiple patients.
Another common mistake is failing to include the attending physician's name. This detail is important for tracking who prescribed the medications. Without this information, it can be difficult to clarify any questions about the medication regimen. Additionally, some individuals neglect to fill in the month and year fields. This oversight can create confusion about when the medication administration is taking place.
People often forget to mark the correct medication hour. Each hour should be checked off clearly to ensure that the medications are administered at the right times. Miscommunication can occur if these hours are not accurately recorded. Similarly, using unclear abbreviations or symbols can lead to misunderstandings. For example, marking “R” for refused or “D” for discontinued should be done with care to ensure that everyone understands what these notations mean.
Another mistake is not recording the medication administration at the time of administration. This is a critical step that helps maintain an accurate record of when medications were given. Skipping this step can lead to discrepancies in the patient's medication history. Additionally, people sometimes forget to document any changes in medication, which should be noted as “C” for changed. Keeping track of these changes is vital for ongoing patient care.
Lastly, some individuals do not double-check their entries. A quick review of the completed form can help catch any errors before they become problematic. Ensuring accuracy in the Medication Administration Record Sheet is not just about following procedures; it directly impacts patient safety and care. By avoiding these common mistakes, caregivers can contribute to a more effective medication administration process.