Do Not Resuscitate Order Document for Georgia
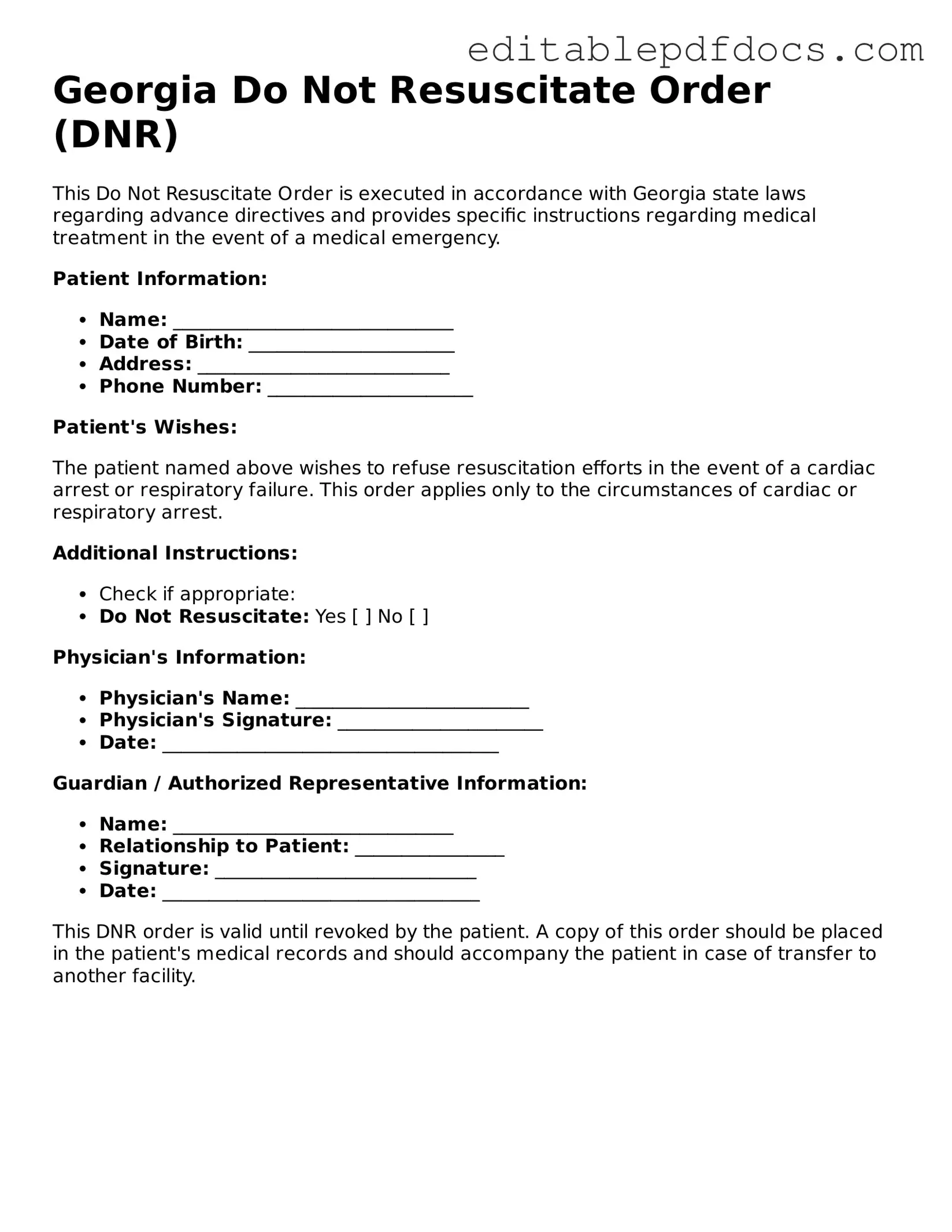
In the state of Georgia, the Do Not Resuscitate (DNR) Order form serves as a crucial legal document that reflects an individual's wishes regarding medical intervention in the event of a cardiac arrest or respiratory failure. This form allows patients to communicate their desire not to receive cardiopulmonary resuscitation (CPR) or other life-saving measures, ensuring that their end-of-life preferences are respected by healthcare providers. It is essential for individuals to understand that a DNR order is not a blanket refusal of all medical treatment; rather, it specifically pertains to resuscitation efforts. To be valid, the form must be properly completed and signed by the patient or their legal representative, along with a physician's signature, confirming that the decision has been made based on informed consent. Additionally, the DNR order must be readily accessible, often kept in a visible location or included in the patient's medical records, to ensure that emergency personnel can easily locate it when needed. Understanding the implications and requirements of the DNR Order form can empower individuals and families to make informed decisions about their healthcare and end-of-life wishes.
File Information
| Fact Name | Description |
|---|---|
| Definition | A Do Not Resuscitate (DNR) Order is a legal document that allows individuals to refuse resuscitation efforts in the event of cardiac or respiratory arrest. |
| Governing Law | The Georgia Do Not Resuscitate Order is governed by Georgia Code § 31-39-1 through § 31-39-7. |
| Eligibility | Any adult can complete a DNR order, and it can also be completed on behalf of a minor by a parent or legal guardian. |
| Signature Requirement | The DNR order must be signed by the individual or their authorized representative, as well as a physician. |
| Form Availability | The Georgia DNR form is available online through the Georgia Department of Public Health and various healthcare facilities. |
| Revocation | Individuals can revoke a DNR order at any time, and this can be done verbally or in writing. |
| Emergency Medical Services | Emergency medical personnel are required to honor a valid DNR order in the event of a medical emergency. |
| Healthcare Provider Responsibilities | Healthcare providers must ensure that the DNR order is documented in the patient's medical record and communicated to all staff involved in the patient's care. |
| Impact on Other Treatments | A DNR order only applies to resuscitation efforts and does not affect other medical treatments or interventions. |
Dos and Don'ts
When filling out the Georgia Do Not Resuscitate Order form, it is crucial to approach the process with care and attention. Here are five things to keep in mind:
- Do ensure you understand the implications of a Do Not Resuscitate Order. This decision affects your medical treatment in emergencies.
- Do consult with your healthcare provider before completing the form. Their guidance can help clarify your options and preferences.
- Do sign and date the form in the presence of a witness. This step is essential for the document to be valid.
- Don't fill out the form under pressure or without fully considering your wishes. Take your time to reflect on your choices.
- Don't forget to provide copies of the completed form to your healthcare provider and family members. Ensure everyone involved is aware of your wishes.
Documents used along the form
The Georgia Do Not Resuscitate Order (DNR) form is an essential document for individuals who wish to express their preferences regarding resuscitation efforts in medical emergencies. Along with this form, several other documents can support and clarify a person's healthcare wishes. Below is a list of these documents, each serving a unique purpose in the realm of healthcare decision-making.
- Advance Directive for Health Care: This document outlines a person's wishes regarding medical treatment if they become unable to communicate. It can include preferences for life-sustaining treatment and appoint a healthcare agent.
- Living Will: A living will specifies the types of medical treatments a person does or does not want in situations where they are terminally ill or permanently unconscious.
- Healthcare Power of Attorney: This document designates an individual to make healthcare decisions on behalf of another person if they are incapacitated. It ensures that someone trusted can advocate for the patient's wishes.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST provides specific medical orders for patients with serious illnesses. It is a more detailed approach than a DNR, addressing various treatment options based on the patient's condition.
- Do Not Intubate (DNI) Order: A DNI order indicates that a patient does not wish to be intubated or placed on a ventilator. This complements a DNR and clarifies the patient's wishes regarding respiratory support.
- Texas RV Bill of Sale: Understanding the Bill of Sale for an RV Purchase can greatly assist buyers and sellers in ensuring legal and proper ownership transfer.
- Patient Care Preferences: This document allows individuals to express their values and preferences about end-of-life care, including pain management and spiritual support, ensuring that their wishes are honored.
- Organ Donation Form: This form indicates a person's wishes regarding organ donation after death. It can provide clarity and direction for healthcare providers and family members during critical moments.
These documents work together to create a comprehensive approach to healthcare decision-making. Having them in place can provide peace of mind for individuals and their families, ensuring that medical care aligns with personal values and preferences.
Consider Some Other Do Not Resuscitate Order Templates for US States
Free Printable Dnr Form - Some hospitals have specific forms for DNR orders that must be used to ensure compliance.
Is a Dnr an Advance Directive - Each state may have specific rules regarding the validity and acceptance of a DNR order.
Polst Form Washington State - May be part of a broader healthcare plan for chronic conditions.
In order to formalize the leasing process and ensure all parties are protected under the law, it's essential for landlords and tenants to utilize a structured framework, which can be found in the Florida Commercial Lease Agreement form. For those looking to begin this process, click here to access the necessary documentation.
Does a Dnr Need to Be Notarized in California - A DNR can reduce unnecessary interventions that may prolong suffering in certain medical scenarios.
Similar forms
A Do Not Resuscitate (DNR) Order is an important document that expresses a person's wishes regarding medical treatment in the event of a life-threatening situation. Several other documents serve similar purposes in guiding healthcare decisions. Here are four documents that are comparable to a DNR Order:
- Advance Healthcare Directive: This document allows individuals to outline their preferences for medical treatment in various situations, including end-of-life care. It can include instructions about resuscitation, making it similar to a DNR Order.
- Living Will: A living will is a specific type of advance directive that details what medical treatments a person does or does not want in the event they are unable to communicate their wishes. Like a DNR, it can specify a person's desire to forgo resuscitation.
- Healthcare Power of Attorney: This document designates a trusted person to make healthcare decisions on behalf of an individual if they become incapacitated. While it does not directly address resuscitation, it empowers the appointed agent to follow the individual's wishes regarding DNR orders and other treatments.
- Employment Verification Form: This document is essential for confirming a candidate's job history and qualifications, aiding employers in making informed hiring decisions. For further details, visit topformsonline.com/.
- Physician Orders for Life-Sustaining Treatment (POLST): A POLST form translates a patient's treatment preferences into actionable medical orders. It is similar to a DNR Order as it clearly states whether a patient wishes to receive resuscitation or other life-sustaining measures.
Understanding these documents is crucial for making informed healthcare decisions. Each serves a unique purpose but ultimately aims to respect the individual's wishes in critical medical situations.
Common mistakes
Completing a Georgia Do Not Resuscitate (DNR) Order form is a crucial step in expressing one’s healthcare preferences. However, many individuals encounter pitfalls that can lead to confusion or even invalidate their wishes. One common mistake is failing to provide the necessary personal information accurately. It’s essential to include the patient’s full name, date of birth, and any other required identifying details. Omitting this information can result in the form being disregarded in a medical emergency.
Another frequent error involves not having the form properly signed. The DNR Order requires signatures from both the patient (or their legal representative) and a witness. Without these signatures, the document may not hold legal weight. Additionally, the witness must be someone who is not related to the patient or involved in their care, which can complicate the process if the wrong person is chosen.
People often overlook the importance of specifying the patient's preferences clearly. The language used in the form should be straightforward and unambiguous. If the instructions are vague, medical personnel may misinterpret the patient’s wishes. It’s advisable to review the wording carefully to ensure that it accurately reflects the intent.
Another mistake is failing to review and update the DNR Order regularly. Life circumstances can change, and so can a person's healthcare preferences. If the form is outdated, it may not align with the patient’s current wishes. Regularly revisiting the document ensures that it remains a true reflection of the individual’s desires.
Some individuals also neglect to discuss their DNR Order with family members or healthcare providers. Open communication about end-of-life wishes is vital. Without these conversations, loved ones may feel uncertain or conflicted during critical moments. It’s essential to ensure that everyone involved understands the patient’s decisions.
Lastly, individuals sometimes fail to keep copies of the DNR Order in accessible locations. Having the document readily available can make a significant difference in emergency situations. It’s advisable to provide copies to healthcare providers, family members, and even keep one in a visible spot at home. This ensures that the patient's wishes are honored promptly and effectively.