Do Not Resuscitate Order Document for Florida
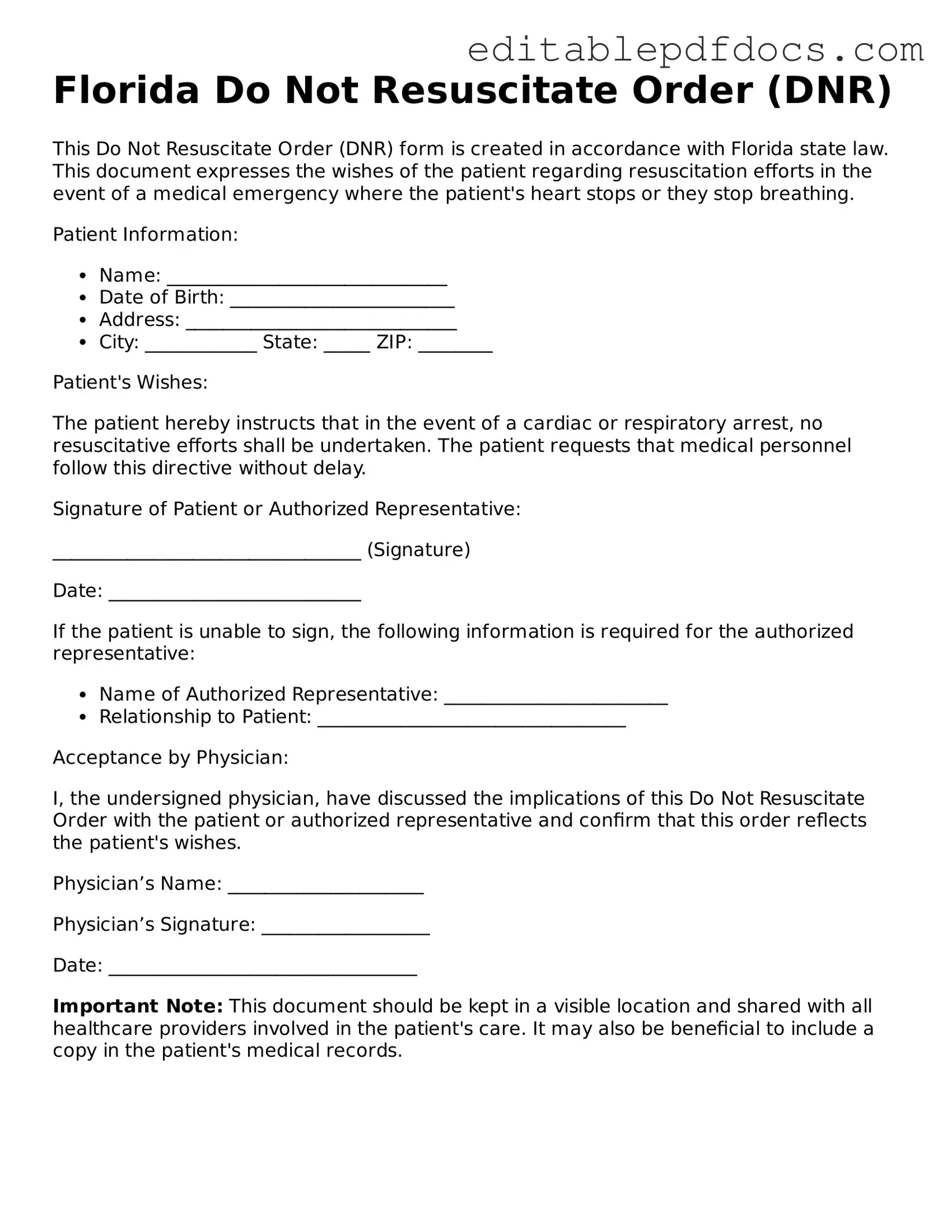
In Florida, the Do Not Resuscitate (DNR) Order form serves as an important legal document for individuals who wish to make their end-of-life care preferences known. This form allows a person to express their desire not to receive cardiopulmonary resuscitation (CPR) or other life-saving measures in the event of a cardiac arrest or respiratory failure. It is designed to ensure that medical professionals respect the wishes of patients who may be facing terminal conditions or irreversible illnesses. The DNR form must be completed and signed by both the patient and a physician, ensuring that the decision is informed and voluntary. Additionally, it is crucial for individuals to discuss their choices with family members and healthcare providers, as this can help avoid confusion during critical moments. Properly completed, the DNR Order becomes part of the patient's medical record, guiding healthcare teams in delivering care that aligns with the patient's values and desires.
File Information
| Fact Name | Description |
|---|---|
| Definition | A Florida Do Not Resuscitate Order (DNRO) is a legal document that allows a person to refuse resuscitation efforts in the event of a medical emergency. |
| Governing Law | The DNRO is governed by Florida Statutes, specifically Section 401.45. |
| Eligibility | Any adult can create a DNRO, provided they are of sound mind and understand the implications of the order. |
| Signature Requirements | The form must be signed by the individual or their legal representative, along with the signatures of two witnesses or a notary public. |
| Form Availability | The DNRO form can be obtained from various sources, including healthcare providers and the Florida Department of Health. |
| Validity | The DNRO remains valid as long as it is properly completed and signed, and it does not have an expiration date unless revoked. |
| Emergency Services | Emergency medical personnel are required to honor a valid DNRO when responding to a medical emergency. |
| Revocation | A DNRO can be revoked at any time by destroying the document or by informing healthcare providers of the decision. |
Dos and Don'ts
When filling out the Florida Do Not Resuscitate Order form, it’s important to approach the process thoughtfully. Here’s a list of things you should and shouldn’t do:
- Do ensure that you understand what a Do Not Resuscitate Order means.
- Do consult with a healthcare professional before making decisions.
- Do discuss your wishes with family members and loved ones.
- Do fill out the form completely and accurately.
- Do sign and date the form in the presence of a witness.
- Don't rush through the form without considering your options.
- Don't assume that your wishes are known without discussing them.
- Don't forget to keep copies of the signed form for your records.
- Don't ignore state laws regarding the completion of the form.
- Don't hesitate to ask questions if you are unsure about anything.
Taking the time to follow these guidelines can help ensure that your wishes are respected and understood.
Documents used along the form
A Florida Do Not Resuscitate Order (DNRO) form is an important document that allows individuals to express their wishes regarding resuscitation in the event of a medical emergency. Alongside the DNRO, several other forms and documents may be relevant in ensuring that a person's healthcare preferences are respected. Below is a list of commonly used documents that complement the DNRO.
- Advance Directive: This document outlines a person's preferences for medical treatment in situations where they cannot communicate their wishes. It can include decisions about life-sustaining treatment, organ donation, and other healthcare choices.
- Healthcare Surrogate Designation: This form appoints someone to make healthcare decisions on behalf of an individual if they become unable to do so. It ensures that a trusted person can advocate for the individual’s medical preferences.
- Living Will: A living will specifies an individual's wishes regarding end-of-life care, particularly in cases of terminal illness or irreversible conditions. It provides guidance to healthcare providers and loved ones about treatment preferences.
- Physician Orders for Life-Sustaining Treatment (POLST): This is a medical order that outlines a patient’s preferences for treatment in emergencies. It is intended for individuals with serious illnesses and is signed by a healthcare provider.
- Mobile Home Bill of Sale Form: To ensure proper documentation in mobile home transactions, refer to the thorough Mobile Home Bill of Sale form guide for a seamless transfer of ownership.
- Do Not Hospitalize Order: This order indicates that a patient does not wish to be hospitalized, even for treatment of acute conditions. It is important for individuals who prefer to receive care at home or in a hospice setting.
- Power of Attorney for Healthcare: This legal document allows an individual to designate someone to make healthcare decisions on their behalf. It is broader than a healthcare surrogate designation and can include financial decisions as well.
- Organ Donation Registration: This document indicates an individual’s wishes regarding organ donation after death. It can be part of an advance directive or a separate registration with a state registry.
These documents work together to ensure that an individual's healthcare preferences are clearly communicated and honored. It is essential to review and update these forms regularly to reflect any changes in personal wishes or health status.
Consider Some Other Do Not Resuscitate Order Templates for US States
Does a Dnr Need to Be Notarized in California - Obtaining a DNR usually involves discussion with healthcare providers to ensure all options are considered.
The completion of the Florida Sales Tax form is essential for businesses operating within the state to ensure compliance with tax regulations. As you prepare to file, it can be helpful to have a detailed understanding of the form's requirements, including how to report gross sales and exempt transactions accurately. For those who need further assistance or want to reference the form directly, you can view the pdf to access all the necessary information and guidelines.
Is a Dnr an Advance Directive - Hospitals may have their own policies regarding the issuance and honoring of DNR orders.
Similar forms
- Advance Healthcare Directive: This document allows individuals to outline their preferences for medical treatment in situations where they cannot communicate. Like a DNR, it provides guidance to healthcare providers about the patient’s wishes.
- Living Will: A living will specifies the types of medical treatment a person wishes to receive or avoid at the end of life. Similar to a DNR, it communicates the patient's desires regarding life-sustaining measures.
- Durable Power of Attorney for Healthcare: This document designates someone to make healthcare decisions on behalf of an individual if they become incapacitated. It can include instructions similar to those found in a DNR.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST is a medical order that outlines a patient’s preferences for treatment, including resuscitation. It is similar to a DNR in that it is intended to guide emergency medical services.
- Employment Verification Form: This document verifies an individual's employment history and status, crucial for confirming qualifications in the hiring process. It can be seamlessly integrated into your workflow by using Fillable Forms.
- Do Not Intubate (DNI) Order: This order specifically instructs healthcare providers not to place a patient on a ventilator. It is a more focused directive that aligns with the principles of a DNR.
- Comfort Care Order: This document emphasizes the provision of comfort and relief from pain rather than curative treatment. It often aligns with the intent of a DNR to avoid aggressive interventions.
- Healthcare Proxy: A healthcare proxy allows an individual to appoint someone to make medical decisions on their behalf. This can include decisions about resuscitation, similar to the intentions behind a DNR.
- Do Not Hospitalize (DNH) Order: This order expresses a patient’s wish to avoid hospitalization in certain circumstances. It can reflect similar values as a DNR regarding the avoidance of aggressive medical interventions.
- End-of-Life Care Plan: This plan outlines the patient’s preferences for care during their final days. It often includes decisions about resuscitation and other life-sustaining measures, paralleling the DNR.
- Patient's Bill of Rights: While broader in scope, this document outlines a patient's rights regarding medical treatment, including the right to refuse treatment, which is a principle underlying the DNR.
Common mistakes
Completing a Florida Do Not Resuscitate Order (DNRO) form is a critical task that requires careful attention to detail. However, many individuals make mistakes that can lead to confusion or complications during a medical emergency. Understanding these common errors can help ensure that your wishes are accurately represented.
One frequent mistake is failing to sign the form. The DNRO must be signed by the patient or their legal representative to be valid. Without this signature, medical personnel may not honor the directive. Always double-check that the form is signed before submitting it.
Another common error is neglecting to date the form. A missing date can lead to questions about the form's validity. It’s important to include the date when the DNRO is signed to confirm that it reflects your current wishes.
Many people also overlook the requirement for a witness. In Florida, the DNRO must be witnessed by two adults who can attest to the signing. If this step is skipped, the form may not be recognized by healthcare providers. Ensure that your witnesses are present and understand their role in this process.
Some individuals fail to specify their preferences clearly. The DNRO form should explicitly state your wishes regarding resuscitation. Ambiguities can lead to misinterpretation during a critical moment. Take the time to fill out the form thoughtfully and clearly.
Additionally, not keeping a copy of the completed DNRO is a common oversight. After filling out the form, it is essential to retain a copy for your records. This ensures that you can provide it to healthcare providers when needed and helps avoid any potential disputes.
Another mistake occurs when individuals do not inform their family members or healthcare providers about the DNRO. It’s crucial that those involved in your care are aware of your wishes. Open communication can prevent confusion and ensure that your preferences are respected.
Some people mistakenly think that a DNRO is a permanent document. In reality, you can change or revoke your DNRO at any time. If your preferences change, be sure to complete a new form and inform your healthcare team.
Finally, many individuals do not consider the implications of the DNRO on their overall healthcare decisions. The DNRO is just one part of advance care planning. It’s beneficial to think about how this decision fits into your broader healthcare goals and discuss it with your healthcare provider.