Fill a Valid Cna Shower Sheets Template
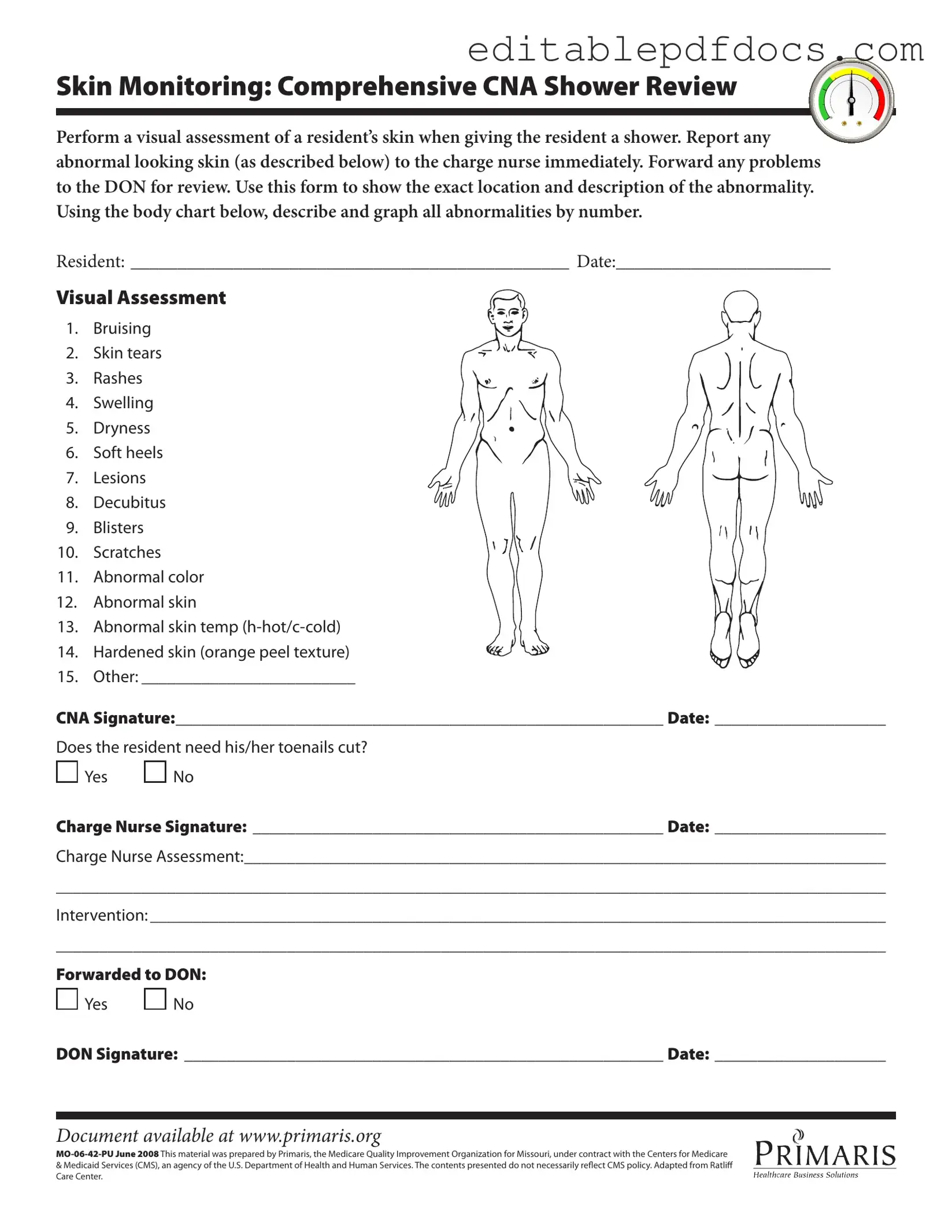
The CNA Shower Sheets form is an essential tool in ensuring the health and safety of residents during their bathing routines. It serves multiple purposes, primarily focusing on skin monitoring, which is crucial for early detection of potential issues. When a Certified Nursing Assistant (CNA) provides a shower, they are tasked with conducting a thorough visual assessment of the resident's skin. This includes identifying any abnormalities such as bruising, skin tears, rashes, or lesions. Immediate reporting of these findings to the charge nurse is vital, as it allows for prompt intervention and care. The form includes a detailed body chart where CNAs can accurately document the location and nature of any skin issues. Additionally, it prompts the CNA to assess whether the resident requires toenail trimming, which can also impact overall skin health. After the initial assessment, the charge nurse reviews the findings, adding their signature and comments, which further ensures a collaborative approach to resident care. Finally, the form includes a section for forwarding information to the Director of Nursing (DON), emphasizing the importance of communication within the healthcare team. This structured process not only enhances the quality of care but also helps in maintaining comprehensive records for each resident.
Document Details
| Fact Name | Description |
|---|---|
| Purpose of the Form | The CNA Shower Sheets form is used to document skin assessments during resident showers, ensuring any abnormalities are reported and addressed promptly. |
| Skin Monitoring | It requires a comprehensive visual assessment of the resident's skin, focusing on identifying issues such as bruising, rashes, and lesions. |
| Reporting Protocol | Any abnormal findings must be reported to the charge nurse immediately, who will then forward the information to the Director of Nursing (DON) for further review. |
| Documentation Requirements | The form includes sections for the resident's information, visual assessment findings, CNA and charge nurse signatures, and any interventions taken. |
| Governing Law | This form is governed by state regulations regarding patient care and documentation standards, specifically under Missouri's health care laws. |
Dos and Don'ts
When filling out the CNA Shower Sheets form, it is important to follow certain guidelines to ensure accuracy and clarity. Here are four things you should and shouldn't do:
- Do: Perform a thorough visual assessment of the resident's skin.
- Do: Report any abnormalities to the charge nurse immediately.
- Don't: Leave any sections of the form blank; complete all required information.
- Don't: Use vague descriptions; be specific about the location and nature of any abnormalities.
Documents used along the form
When caring for residents, it's important to have the right forms and documents to ensure proper communication and record-keeping. The CNA Shower Sheets form is just one piece of the puzzle. Below are other essential forms that are often used alongside it.
- Resident Care Plan: This document outlines the specific needs and preferences of each resident. It includes goals for care and strategies to achieve those goals, ensuring that all staff members are on the same page regarding the resident's care.
- Divorce Settlement Agreement: This document outlines the terms of a divorce, ensuring a fair distribution of assets and responsibilities; the form is available here.
- Incident Report: If any unusual events occur during care, such as a fall or injury, an incident report is filled out. This form helps document what happened, when it happened, and the actions taken afterward, which is crucial for improving safety and care practices.
- Daily Progress Notes: Caregivers use this form to record daily observations and interactions with residents. It provides a snapshot of each resident's condition and any changes that may need attention, making it easier to track their overall health.
- Skin Assessment Form: This form is specifically for documenting skin conditions. It allows caregivers to note any changes in skin integrity over time, helping to prevent issues like pressure ulcers and ensuring timely interventions.
- Medication Administration Record (MAR): This document tracks the medications given to residents. It includes details about dosages, timing, and any reactions, ensuring that residents receive their medications safely and as prescribed.
- Consent Forms: These forms are used to obtain permission from residents or their families for various treatments and procedures. They ensure that caregivers have the legal right to provide care and that residents understand what they are consenting to.
Using these documents together with the CNA Shower Sheets form helps create a comprehensive care approach. Proper documentation is key to maintaining high standards of care and ensuring the well-being of all residents.
Popular PDF Forms
Schedule C 1040 - The form aids in budgeting and financial forecasting.
Free Lease Agreement Florida Template - Guidelines for hosting guests are established to avoid disturbances in the community.
The Free And Invoice PDF form not only simplifies invoicing for both individuals and businesses but also allows users to access valuable resources online. For more information, visit topformsonline.com/, where one can find templates and further guidance on creating professional invoices that ensure financial clarity and promote timely payments.
Irs Form 14653 - Taxpayers are required to elaborate on the specific factors that led to their non-compliance.
Similar forms
-
Incident Report Form: Similar to the CNA Shower Sheets, this document records specific events or abnormalities observed during care. Both forms require detailed descriptions and prompt reporting to supervisors, ensuring that any issues are documented and addressed quickly.
-
Skin Assessment Form: This form focuses on evaluating a resident's skin condition, much like the CNA Shower Sheets. Both documents require a systematic approach to identify skin issues, including rashes, bruises, and lesions, to ensure proper care and treatment.
- Boat Bill of Sale: The Fillable Forms provide a streamlined way to create this essential document, which officially records the ownership transfer of a boat in California, ensuring both parties are protected in the transaction.
-
Care Plan Update Form: Similar to the CNA Shower Sheets, this document is used to record changes in a resident’s condition and to adjust their care plan accordingly. Both forms facilitate communication among healthcare staff about the resident's needs and any interventions required.
-
Daily Progress Notes: This document captures the daily observations and changes in a resident's condition, akin to the CNA Shower Sheets. Both require documentation of specific findings and any necessary follow-up actions, promoting continuity of care.
Common mistakes
Filling out the CNA Shower Sheets form accurately is crucial for the well-being of residents. However, several common mistakes can lead to incomplete or inaccurate information. One major error is failing to conduct a thorough visual assessment of the resident's skin. Skipping this step can result in overlooking serious conditions that require immediate attention.
Another frequent mistake is not documenting the specific location of any abnormalities. When abnormalities are noted, it is essential to pinpoint where they occur on the body chart provided. Vague descriptions can lead to confusion and hinder proper follow-up care.
Many individuals also forget to report findings to the charge nurse promptly. Delays in communication can exacerbate health issues. It is vital to notify the charge nurse immediately after identifying any skin concerns, ensuring that the resident receives timely intervention.
Inaccurate descriptions of skin conditions pose another challenge. For instance, using terms like "red" or "sore" without further detail does not provide sufficient information. Instead, clear and specific descriptions help medical professionals understand the severity and type of issue.
Some CNAs neglect to indicate whether the resident needs toenail care. This oversight can lead to further complications, especially for residents with mobility issues or diabetes. It is important to assess and document this need as part of the overall care plan.
Failing to obtain the charge nurse's signature is another common mistake. This signature serves as confirmation that the findings have been reviewed and acknowledged. Without it, the documentation may not hold the necessary weight in the care process.
Additionally, some CNAs do not forward the completed form to the Director of Nursing (DON) when required. This step is crucial for ensuring that any serious skin issues are escalated and addressed appropriately. Neglecting this can hinder the overall quality of care provided to residents.
Lastly, not keeping a copy of the completed form for personal records can lead to issues down the line. Having a reference can be invaluable for continuity of care and for any follow-up discussions with nursing staff. Maintaining thorough documentation is essential for effective communication and quality care.