Fill a Valid Annual Physical Examination Template
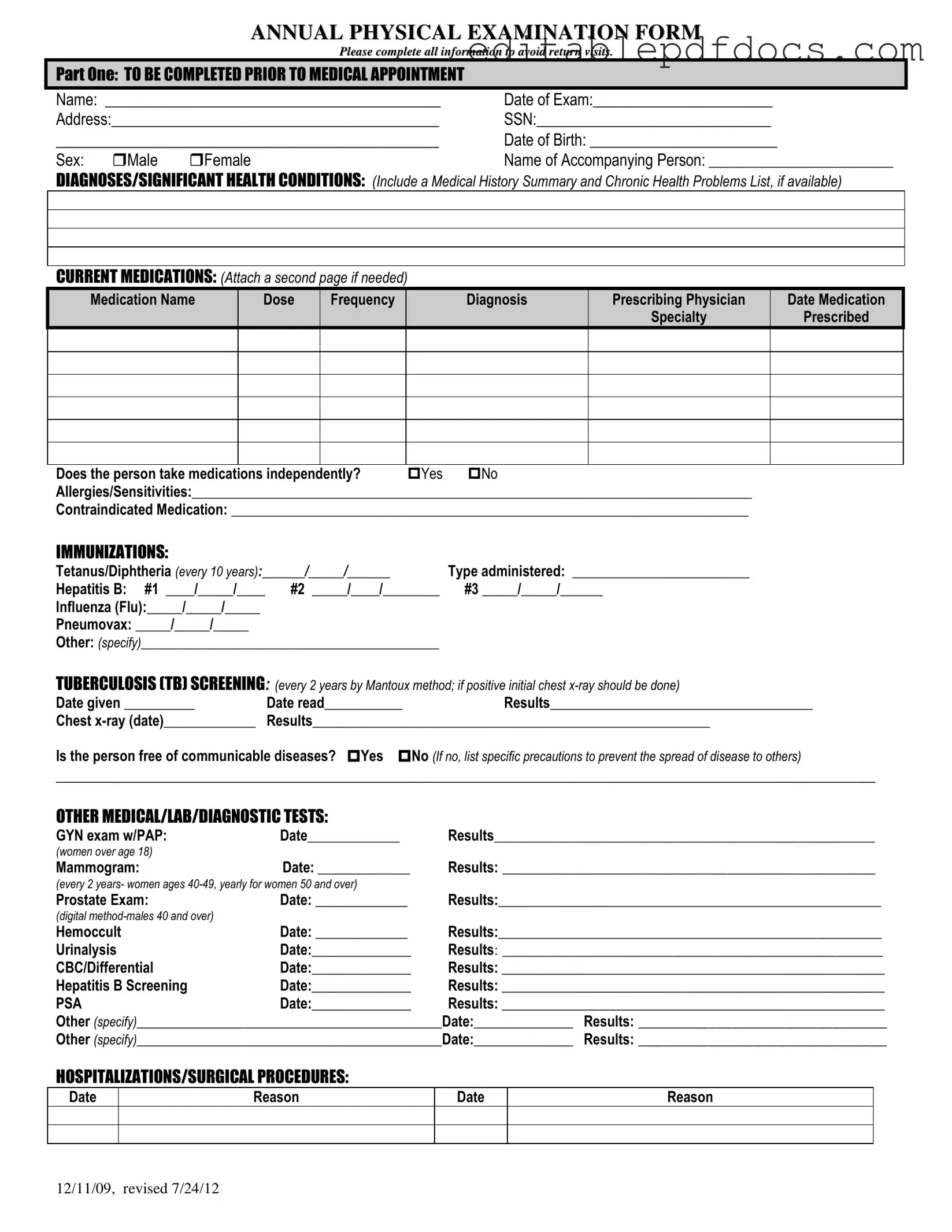
The Annual Physical Examination form serves as a comprehensive tool designed to gather essential health information from individuals prior to their medical appointments. This form includes multiple sections that require the completion of personal details, such as name, date of birth, and address, ensuring that healthcare providers have accurate records. It prompts patients to disclose significant health conditions, current medications, and any allergies or sensitivities they may have, which is crucial for safe and effective treatment. Immunization history is also documented, covering vaccines like Tetanus, Hepatitis B, and Influenza, alongside any tuberculosis screening results. Additionally, the form captures data on past hospitalizations and surgical procedures, providing a fuller picture of the patient’s medical history. The physical examination section includes vital signs and evaluations of various body systems, allowing for a thorough assessment of the individual’s overall health. Recommendations for health maintenance, dietary guidelines, and any necessary follow-up evaluations are also noted, ensuring that patients receive personalized care tailored to their specific needs. Overall, this form not only facilitates effective communication between patients and healthcare providers but also plays a vital role in promoting proactive health management.
Document Details
| Fact Name | Details |
|---|---|
| Purpose | The Annual Physical Examination form is designed to collect comprehensive health information before a medical appointment. |
| Required Information | Patients must provide personal details such as name, date of birth, and medical history to ensure accurate assessment. |
| Medication Disclosure | Current medications must be listed, including dosage and prescribing physician, to inform treatment decisions. |
| Immunization Records | Patients are required to document their immunization history, including dates for vaccines like Tetanus and Hepatitis B. |
| Health Screening | Screenings for conditions such as tuberculosis and prostate health are included, with specific recommendations based on age and gender. |
| Legal Compliance | In some states, the form may be governed by specific health laws requiring its use for certain populations, such as children or the elderly. |
| Physical Examination | A general physical examination section captures vital signs and evaluations of various body systems to assess overall health. |
| Follow-Up Recommendations | Recommendations for ongoing health maintenance, including lab work and lifestyle changes, are provided based on the examination findings. |
Dos and Don'ts
When filling out the Annual Physical Examination form, consider these important dos and don'ts to ensure a smooth process.
- Do complete all sections of the form to avoid delays.
- Do provide accurate personal information, including your name and date of birth.
- Do list all current medications, including dosage and frequency.
- Do mention any allergies or sensitivities clearly.
- Do keep a record of your immunization dates and types.
- Don't leave any sections blank; incomplete forms may lead to return visits.
- Don't forget to sign and date the form before submitting it.
- Don't provide vague information; be as specific as possible.
- Don't rush through the form; take your time to ensure accuracy.
Documents used along the form
When preparing for an annual physical examination, several other forms and documents may be needed to ensure a comprehensive assessment of health. Each document serves a specific purpose and helps healthcare providers gather essential information about a patient’s medical history and current health status. Below is a list of common forms often used alongside the Annual Physical Examination form.
- Medical History Questionnaire: This form collects detailed information about a patient's past medical issues, surgeries, allergies, and family health history. It helps the physician understand the patient's background and any potential risks.
- Medication List: A document listing all current medications, including dosages and frequency. This helps doctors review medication interactions and ensure safe prescribing practices.
- Immunization Record: A summary of vaccinations a patient has received. This record is crucial for assessing a patient's immunity and determining if any additional vaccines are needed.
- Consent for Treatment: A form that patients sign to give healthcare providers permission to perform examinations and procedures. It ensures that patients are informed about their treatment options.
- Release of Information Form: This allows healthcare providers to share a patient’s medical information with other entities, such as specialists or insurance companies, as needed for care or billing.
- Lab Test Requisition: A form used to request specific laboratory tests. It provides necessary details to the lab, ensuring accurate testing and results.
- Referral Form: This document is used when a primary care physician refers a patient to a specialist. It includes relevant medical information to assist the specialist in providing care.
- Health Insurance Information: A form that collects details about a patient’s health insurance coverage. This information is important for billing and understanding coverage for services.
- Employment Verification Form: This important document verifies an individual's employment status and history, providing necessary proof for potential employers during the hiring process. For more details, you can refer to Fillable Forms.
- Advance Directive: A legal document that outlines a patient’s wishes regarding medical treatment in case they become unable to communicate those wishes. It is essential for ensuring that a patient’s preferences are respected.
- Physical Activity Readiness Questionnaire (PAR-Q): This form assesses whether individuals can safely engage in physical activity. It identifies any health concerns that might require medical clearance before starting an exercise program.
Having these forms ready can streamline the annual physical examination process, making it easier for healthcare providers to deliver the best care possible. Each document contributes to a holistic view of a patient’s health, ensuring that all aspects are considered during the examination.
Popular PDF Forms
Artist Performance Agreement - The number of musicians and crew involved in the performance should be indicated.
Joint Tenancy in California - Understanding the nature of joint tenancy is crucial when utilizing this affidavit.
Understanding the importance of the Florida Do Not Resuscitate Order form is essential for individuals who want to make clear decisions regarding their healthcare. By filling out this legal document, they can ensure their preferences are honored in critical situations, as it explicitly instructs healthcare providers not to perform CPR if a person's breathing or heart ceases. For further details on the form and its implications, you can see the document.
Can One Parent Take a Child on a Cruise Royal Caribbean - Having the completed form readily available may streamline travel logistics.
Similar forms
The Annual Physical Examination form shares similarities with several other important documents that also gather health information. Here are four such documents:
- Patient Intake Form: Like the Annual Physical Examination form, the Patient Intake Form collects essential personal information, medical history, and current medications from patients. This document is often filled out before a first visit to a healthcare provider, ensuring that the provider has a comprehensive understanding of the patient's health background.
Mobile Home Bill of Sale: This legal document records the sale and transfer of ownership of a mobile home, ensuring clarity on the terms and conditions for both parties. For more details, please visit https://nyforms.com/mobile-home-bill-of-sale-template.
- Medical History Questionnaire: This document is similar in that it focuses on a patient’s past and current health conditions. It typically asks about previous illnesses, surgeries, and family health history, providing a broader context for the healthcare provider to assess the patient’s health risks and needs.
- Immunization Record: The Immunization Record is akin to the Annual Physical Examination form in that it tracks vaccinations and immunization dates. This document is crucial for ensuring that patients are up-to-date with their vaccinations, similar to how the Annual Physical Examination form includes immunization history as part of the overall health assessment.
- Follow-Up Visit Summary: After a medical appointment, a Follow-Up Visit Summary serves as a record of the findings and recommendations made during the visit. It often includes information about tests performed and medications prescribed, paralleling the detailed evaluations found in the Annual Physical Examination form.
Common mistakes
Filling out the Annual Physical Examination form accurately is essential for ensuring a smooth medical appointment. However, many individuals make common mistakes that can lead to delays or complications. One frequent error is incomplete personal information. Failing to provide full names, addresses, or social security numbers can result in the form being returned for corrections. It is crucial to double-check that all sections are filled out completely before submission.
Another mistake often seen is neglecting to update medical history. Individuals sometimes forget to include recent diagnoses or changes in health conditions. This omission can hinder the physician's ability to provide appropriate care. Always ensure that the medical history section reflects the most current information.
Many people also overlook the current medications section. Listing medications incorrectly or forgetting to mention them can lead to dangerous interactions or inadequate treatment plans. If more space is needed, attaching an additional page is advisable. This ensures that the healthcare provider has a comprehensive view of all medications being taken.
Allergies and sensitivities are another area where errors can occur. Some individuals may fail to disclose all relevant allergies, which can be critical information for the physician. This section should be filled out thoroughly to avoid any adverse reactions during treatment.
In the immunizations section, it is common for individuals to forget to list all vaccinations received. Missing this information can delay necessary immunizations or lead to unnecessary repeat vaccinations. Keeping an updated record of immunizations is beneficial for this reason.
Another frequent oversight is in the evaluation of systems section. People may skip this part or answer inaccurately, leading to potential misdiagnosis. It is important to carefully consider each system and provide honest answers about any symptoms or issues.
Lastly, individuals often neglect to include additional comments or recommendations for health maintenance. This section allows for personalized notes that can guide the physician in providing tailored advice. Ignoring this opportunity can result in missed recommendations that could improve health outcomes.